Treatments
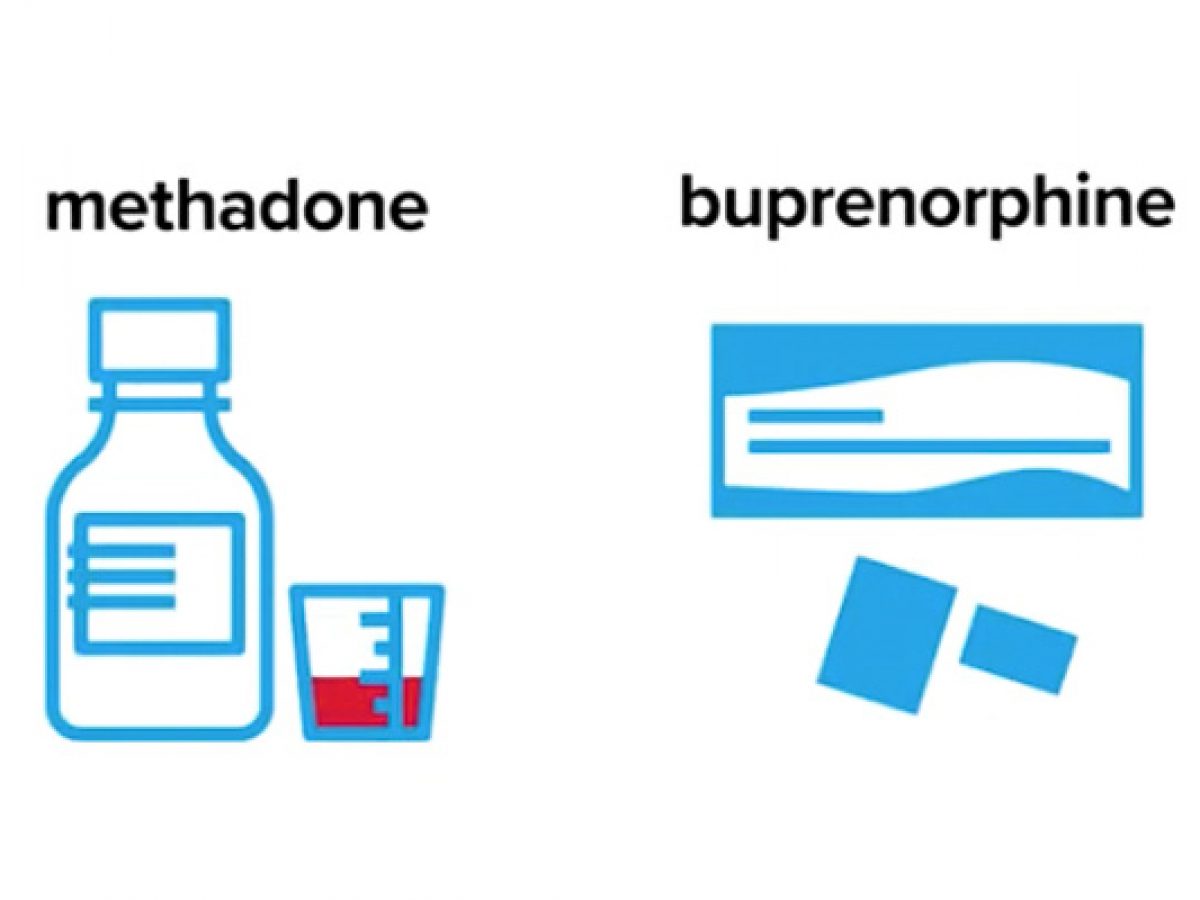
1. Opioid agonist therapy
Methadone and Buprenorphine are used to treat severe pain and opioid addiction. They are long-acting opioids used to replace the short-acting opioids that someone may be addicted to. The effects last for 24 to 36 hours whereas people taking short-acting opioids need to take the drugs 3 to 4 times a day in order to avoid withdrawals. Taken at the correct doses these will prevent withdrawal symptoms and reduce drug cravings. Methadone is a long-term treatment and is available as a tablet or oral solution. When buprenorphine is used to treat pain it is given in patch form to provide relief for 7 days. When buprenorphine is used to treat opioid addiction it is combined with naloxone, usually given in pill form that is absorbed under the tongue (sublingual). Naloxone can cause withdrawal if it is injected, adding it to buprenorphine prevents people from misusing the drug.
Side effects of both drugs include:
- Constipation
- Excessive sweating
- Dry mouth
- Changes in sex drive
- Drowsiness
- Light-headed
- Nausea
- Vomiting
- Weight gain
2. Addiction treatment counselling
Outpatient behavioural treatment: different forms of behavioural therapy for individual or group drug counselling on a regular schedule include…
- Cognitive-behavioural therapy: Helps patients recognize, avoid and cope with situations where they are most likely to use opioids
- Multidimensional family therapy: Used for adolescents as well as their families with opioid abuse to address their drug abuse patterns in order to improve overall family
- Functioning Motivational interviewing: To encourage people to change their behaviour and enter treatment
- Motivational incentives (contingency management): Using positive reinforcement to encourage self-restraint from drugs
Inpatient or residential treatment: different forms of inpatient therapy for individuals with severe problems that need 24-hour intensive care, safe housing and, medical attention include…
- Therapeutic communities: Very structured program where patients remain at a residence for 6-12 months and the community and staff act as influences to change patients attitudes, understanding, and behaviour with drugs
- Shorter-term residential treatment: Focuses on detoxification and providing initial intensive counselling and preparation for community-based treatment
- Recovery housing: Short-term housing following inpatient treatment is used to help people gain independence
3. Naloxone kit

When someone is experiencing an overdose the first step is to give them naloxone. Naloxone kits can be purchased at pharmacies, provincial correctional facilities and the community based-organizations listed below.
- Needle Exchange/Syringe Programs
- Hepatitis C Programs
- Public Health Units
- Aboriginal Health Access Centres
- AIDS Service Organizations
- community health centres
- outreach programs
- withdrawal management programs
- shelters
- hospitals with an emergency department or urgent care centre
What to do When Someone Overdoses

How to Safely Use Opioids
Only take medication prescribed to you and if prescribed opioids talk to your doctor, dentist, or pharmacist on the risk and benefits of the drug. Don’t take opioids with other depressants as opioids are depressants and slow down the part of the brain that controls breathing. Return any unused medication to the pharmacy and do not use other people prescribed medication. Do not use opioids alone but if you do have someone check in on you. Ask others what they are experiencing with the same drug and batch. Check what’s in your drugs at a local drug checking service and always have naloxone on you. Using a supervised consumption service provides a safe and clean environment under qualified supervision for people to take opioids.
Prevention
Educating physicians and patients more often on the severity of opioids. Physicians conduct an initial assessment of the patient and continuous patient monitoring until their prescription is done. Provide patients with educational and training sessions for proper use, storage, and disposal of opioids. Locating inappropriate prescribing of opioids by having a database that identifies mismatches between diagnoses and medication/dose. Pharmacists check patient photo identification to see if it matches the name on the prescription.
Click the link below to find places to receive help


